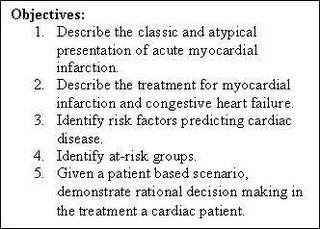
The following is an excerpt from my Clinical Decision Making lecture series on cardiac emergencies. In this selection I focus on the “nuts and bolts” of chest pain and congestive heart failure. The continuation module; SYNCOPE: The EMS Fatal Masquerade will be published shortly.
Previous Clinical Decision Making lectures include LOCATE the Patient and The Dead: Clinical Decision Making in Cardiac Arrest. The latter are under revision and will be re-issued in January 2006.
Cardiac Events and Congestive Heart Failure
It comes as no surprise to the experienced EMT or paramedic that a majority of patients requesting emergency medical service have complaints of cardiac or respiratory nature. These complaints are often categorized from the acute complaint of chest pain, syncope (or near-syncope), or short of breath to cardiac arrest. Most often, when someone calls EMS, there is little question as to what the problem is…especially when the chief complaint is stated as above. Difficulties arise when the chief complaint is less evident and patient presentation is less than acute as in the case of the “weak and dizzy”, the elder person who is just “not acting normal”, and the cold/flu patient.
The difficulty is for the provider to differentiate between the two and treat appropriately. Making the call between myocardial infarction, congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD), and cold/flu can be difficult in any setting. Mistaking the patient in CHF for one who has respiratory infection can be deadly. Equally so, is the patient with syncope or near-syncope that claims to be “fine” now. Conducting a through assessment is critical to discovering what type of condition the patient may have, formulating a differential diagnosis list, and making treatment/transport decisions.
Chest Pain
Discovering the etiology or cause of chest pain can be difficult for EMS providers mainly because the pain is described in vague terms. Patients with cardiac related pain or discomfort often have visceral pain. A patient with visceral pain may complain that the symptoms are located in a general area and intermittent yet, worsen with time. They also note the nature of the pain as dull, aching, or numbness. By contrast, somatic pain is able to be localized to a specific area by the patient. This somatic pain may change with movement or position of the patient. A word of caution is due here; any pain in the chest, either somatic or visceral, must be taken seriously as a potential cardiac event. Fundamental BLS care including oxygen and evaluation by advanced life support is necessary.
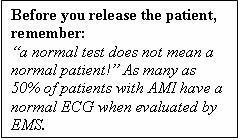
In addition to the quality (visceral or somatic) of pain, the location of chest pain is also non-diagnostic. That is; the location of pain often will not directly relate to the origin of the pain. Many groups of patients may not experience the “classic” symptoms of chest pain, shortness of breath (SOB), arm/neck pain, nausea, diaphoresis, and the like. Diabetics, elderly, and post-menopausal women may experience altered or atypical presentation of a cardiac event. Persons who are chronic drug abusers may also not report textbook symptoms. In any case, decreased severity or absence of pain does not equate to a non-life threatening condition in the setting of chest pain. In addition to the classic signs and symptoms of cardiac events, be on the lookout for the following list in addition to the classic symptoms:
· Weakness and fatigue
· Pressure in the chest
· Palpitations, or racing heart
· SOB or dypsnea…even if mild
· Painful digestion, dydpepsia
· Neck, back and epigastric pain
· Symptoms that wake the patient from sleep or keep them from sleeping
· Any change in mental status, syncope or near-syncope…even if the patient “is fine now”.
Any one of the above should indicate potential for a cardiac event, with or without chest pain. With these complaints, the EMT must consider acute myocardial infraction (AMI), angina (stable and unstable), cardiac dysrhythmias, and pulmonary embolism. Again, solid BLS care should be initiated as well as ALS assessment and transport.
Congestive Heart Failure
Congestive heart failure or CHF is a situation when one or both (univentricular and biventricular) of the heart ventricles is no longer capable of maintaining discharge capacity of fluid returning to the heart. The results may be seen in the form of any number of symptoms depending upon what side of the heart is failing.
This is a good time to remember some basic physiology of the heart. The right side of the heart is under low pressure in relation to the left heart as it receives blood from the body (pre-load) and is responsible for pumping into the pulmonary system for gas exchange. With this in mind, one can visualize that any factor the restricts or diminishes the right heart ability to push blood will result in a backup of fluid into the systemic circulation; the liver and dependant areas for example. This situation is compounded by inability to get blood to the pulmonary system for oxygenation. When this occurs, not only is oxygenation impaired with resulting hypoxemia, but the left ventricle (and cardiac output) also becomes challenged. Simply put, the left heart cannot pump required volume if that volume is not delivered (no pre-load, no after-load). These situations can arise from AMI, valve failure (tricuspid, pulmonary, or both), and fluid depletion. Paradoxically, the most common cause of right heart failure is left heart failure a.k.a Cor Pulmonale.
A similar situation occurs if the left or high pressure side of the heart is involved. The left heart can be thought of as the high pressure side and is responsible for ejecting blood to the body via the aortic valve and the aorta. This is known as after-load. Anything that reduces the left ventricles efficiency can technically cause left heart failure. Think of it this way:
If volume entering the left atria are insufficient, there will be decreased discharge
If the mitral (bicuspid) valve fails either by stenosis or regurgitation (narrowing or allowing backward flow), the left ventricle (LV) either cannot fill or losses discharge pressure and volume back to the left atria.
If the aortic valve is stenosed or narrowed, the LV must work harder to discharge the needed volume and pressure.
If the LV is damaged from AMI and not able to accommodate the preload being sent
These bullets indicate that LV failure can come from any number of causes: AMI, valve failure, and prolonged high systemic pressures (high blood pressure). Regardless of the cause, the results of decreased cardiac output and backup into the pulmonary system (high pulmonary pressures and pulmonary edema) may be seen.
Common Sense Stuff
Heart failure is basically a theory of backed-up fluid that accumulates behind the chamber (or side) of the heart that is affected. Patients with severe left ventricular infarction often exhibit symptoms of respiratory distress and hypoxia as a result of impaired pumping ability (decreased after load) and pulmonary edema as the existing pre load backs up behind the left ventricle. The increased pulmonary pressure is passed on the right ventricle and may eventually cause it to become impaired. In the setting of right heart failure, either resulting from left heart failure or right ventricular AMI, pre load decreases (remember: the left heart can’t pump out what it doesn’t get) and fluid backs up behind the right heart and into the systemic circulation. This fluid accumulation becomes visible as ankle edema, edema in dependant areas of the body, and liver engorgement (congestive hepatomegaly).
Is It Acute or Chronic?
We may find any number of symptoms of heart failure presented to the EMS provider. Unfortunately, the early or mild symptoms may be confused for cold/flu symptoms…a dangerous clinical assessment mistake! The symptoms depend not only on the side of the heart affected, but the rate at which pathology develops. Look at it this way; if a patient suffers a massive MI, arrhythmia such as rapid atrial fibrillation/ventricular tachycardia, or valve failure, drastic reduction of cardiac output and/or pulmonary edema may follow. If the patient goes on to survive any of the above or if conditions progress over a long period of time, the patient may compensate. Compensatory mechanisms may include enlargement of the heart, and many form of neurohormonal changes. In this case frequency of EMS contact and ED visits often increased.
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.